A Scientific Understanding of Chronic Gastritis: Winning the Battle for Your Stomach's Health
- MedBridge NZ
- Oct 2, 2025
- 3 min read
Chronic gastritis is one of the most common stomach ailments, a condition that many of us will encounter at some point in our lives. It acts as a silent alarm, initially presenting with mild symptoms like upper abdominal pain or bloating. However, if left unaddressed, it can lead to more severe health issues. This article will provide a scientific overview of chronic gastritis and guide you on how to manage it effectively.
Chronic Gastritis: A Persistent Battle in Your Stomach Lining
The Mechanism: An Imbalance of Damage and Repair
The gastric mucosa is the natural barrier that protects your stomach wall. When factors such as Helicobacter pylori (H. pylori) infection, long-term medication use, or bile reflux repeatedly attack this lining, the stomach's self-repair capabilities can become overwhelmed, leading to chronic inflammation.
Key Causes:
Helicobacter pylori (H. pylori) Infection: Approximately 70% of chronic gastritis cases are linked to this bacterium, which embeds itself in the stomach lining and releases toxins that cause inflammation.
Medication-Induced Damage: Long-term use of drugs like aspirin and ibuprofen can weaken the protective mechanisms of the gastric mucosa.
Unhealthy Lifestyle Habits: Excessive alcohol consumption, smoking, a high-salt diet, and high levels of stress can all exacerbate damage to the stomach lining. For those considering treatment options abroad, exploring Medical Tourism China can provide access to specialized medical care.
Superficial vs. Atrophic Gastritis: Understanding the Depth of Inflammation
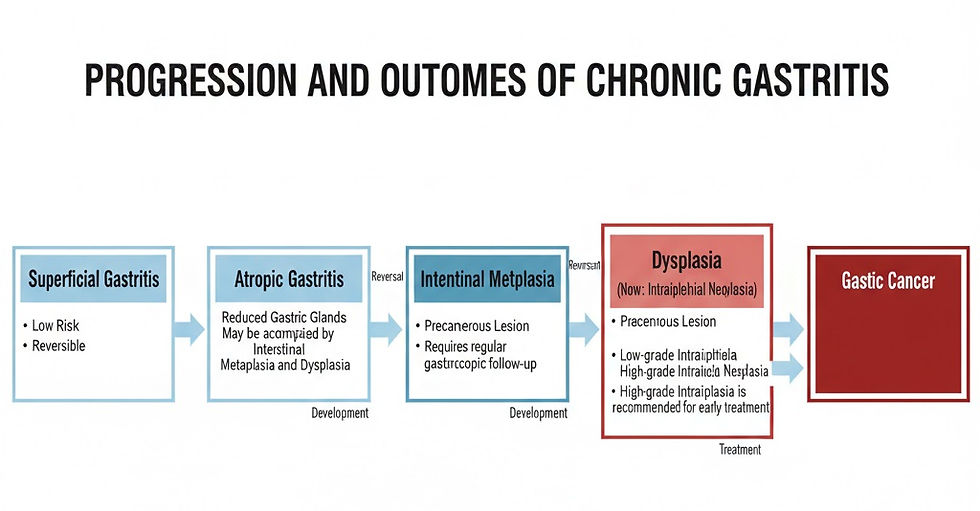
Chronic gastritis is classified into two types based on the severity of the condition, each with different risks and management strategies:
Superficial Gastritis: Inflammation is confined to the surface layer of the gastric mucosa. This is a low-risk, reversible condition.
Atrophic Gastritis: Characterized by a reduction in gastric glands and a thinning of the mucosal layer. This condition carries a higher risk of developing into cancer and requires careful monitoring.
While symptoms for both can be similar (e.g., upper abdominal discomfort, belching), atrophic gastritis may also be accompanied by a loss of appetite and anemia due to reduced iron absorption from decreased stomach acid. It is important to note that "atrophic gastritis" refers to a reduction in glands, not a "shrinking stomach," and timely intervention can slow its progression.
Intestinal Metaplasia: An Unwelcome Guest in the Stomach
When the gastric mucosa is damaged over a long period, some cells may transform into intestinal-like epithelial cells, a condition known as intestinal metaplasia. This is a precancerous state, and while it doesn't mean you have cancer, it requires regular monitoring through gastroscopy.
Intraepithelial Neoplasia: The Final Warning
Intraepithelial neoplasia (previously known as dysplasia) refers to abnormal structural changes in the cells of the gastric mucosa. It is classified as either low-grade or high-grade. High-grade neoplasia is considered a precancerous lesion and requires immediate treatment, often through endoscopic resection or surgery.
Treatment Principles: Addressing the Root Cause
The treatment of chronic gastritis requires a comprehensive approach:
Eradicate H. pylori (Crucial!): The standard treatment is a "quadruple therapy" regimen, which includes a proton pump inhibitor (e.g., omeprazole), two antibiotics, and a bismuth agent, for a course of 10-14 days. Eradicating H. pylori can, in some cases, reverse intestinal metaplasia and reduce the risk of cancer.
Protect the Gastric Mucosa: Medications such as teprenone and rebamipide can help repair the stomach lining.
Symptomatic Treatment: Proton pump inhibitors for acid reflux and prokinetic agents for bloating.
Lifestyle Adjustments: Eat smaller, more frequent meals, avoid pickled, fried, and overly hot foods, quit smoking, limit alcohol, and manage stress.
For international patients seeking treatment, a medical concierge provider can assist in coordinating appointments, managing travel logistics, and ensuring a seamless healthcare experience.
Gastroscopy Follow-Up: Keeping Risks in Check
Regular monitoring is key to managing chronic gastritis:
Atrophic Gastritis (without intestinal metaplasia or neoplasia): Every 2-3 years.
Atrophic Gastritis with Intestinal Metaplasia: Every 1-2 years.
Low-Grade Intraepithelial Neoplasia: Every 6-12 months.
High-Grade Intraepithelial Neoplasia: Immediate treatment.
Prevention: Creating a Gentle Environment for Your Stomach
Block Infection Sources: Use serving utensils when dining with others to prevent the spread of H. pylori.
Eat Smart: Consume plenty of fresh fruits and vegetables and consider adding probiotics to your diet.
Don't Ignore Pain Signals: If you experience persistent upper abdominal discomfort, seek medical attention promptly.
Conclusion
Chronic gastritis is a health reminder from your body. Through proactive management, including eradicating H. pylori, regular follow-ups, and lifestyle adjustments, you can effectively control the risks. Remember, the well-being of your stomach is in your hands.
This article was written by Dr. Chen Li, Chief Physician, from the Department of Gastroenterology at Shanghai Ruijin Hospital.



